Traditional Chinese Medicine (TCM) has a long and rich history, and is the third oldest form of medicine. Only Egyptian and Babylonian medicine predates it. The fact that TCM has existed for thousands of years, and is still used today is a testament to its value as a form of healthcare.  |
Hanging Gardens of Babylonia ( 3500B.C.) |
|
|
 |
Egyptian medicine man
(3000BC) |
The isolation of China throughout history plays a role in TCM's lack of development in other world civilizations. However, with the opening of China in 1972 it has been spreading to Western and European countries. TCM's practice has been shaped over time by many factors including culture, philosophy, politics, religion, and science.
Today, we think of China as being one united country, but this is only a recent development in the country's history. Throughout the centuries, China was made up of many states that were often at war with each other and repeatedly united and divided. These states were ruled by dynasties and were feudalistic societies.
 |
Map of China |
Development of TCM, therefore, was not always a sequential build up of knowledge based on the previous dynasty's contributions. How the individual practiced TCM was influenced largely by his teacher's views. Even today, we see these differences. For example, different TCM practitioners may prescribe a person with the same symptoms different herbal remedies. Each herbal remedy will cure the symptoms even though they have different ingredients. The success of the treatment is measured through observation and how the patient feels. Traditional Chinese medicine plays a very important part in medicine's history. Understanding TCM through a historical context gives insight to this ancient form of medicine and establishes its validity as a healthcare system.Qin Dynasty 221 - 207 BC
Emperor Qin Shi Huangdi |
| About the Qin
Emperor Qin Shi Huangdi was the first emperor to unite China. He did this not only through force, but also by standardizing systems throughout the country such as currency, writing, weights and measurements. His policies were strict and many nobles and scholars disliked them. He put 460 scholars to death as a warning to those who considered opposing them. His most infamous act was the "burning of the books " in 213 BC. As a result, many important writings from ancient China were lost. Fortunately some texts on divination,
 | | Burning books and burying scholars alive |
medicine and agriculture were saved. Eventually his empire fell apart with the uprising of the peasants that led to the founding of the Han Dynasty. |
Han Dynasty 206 BC - 220 AD* Western Han 206 BC
-24 AD
* Eastern Han 25
-220 AD
About the HanLiu Bang launched the Han Dynasty in 206 BC and adopted the systems and harsh laws initially put in place by Emperor of the Qin Dynasty. During the years of 9 to 23 AD,
Wang Man founded a new dynasty called the Xin, which marked a break between the Western and Eastern Han. However, his reign was short lived and in 23 AD a rebel peasant army, the Red Eyebrows put Wang Mang to death signaling the beginning of the Eastern Han Dynasty.
 |
| Expanded empire of Western Han Dynasty |
During this period, nomadic tribes were constantly invading China. As a result the Western Han Dynasty expanded its empire into what is today known as Mongolia, Manchuria, Korea, South China, Vietnam, and Central Asia. The Silk Road in Northwest China was a popular communication and trade route. The Han dynasty was also a time of innovation with vast developments in the arts, philosophy and technology. For example, Zang Heng (78-139AD), a scientist and astronomer, invented the first seismograph in the 2nd century.
The Role of Philosophy and Religion Philosophy, societal values and religion played key roles in shaping the practice of Chinese medicine. Many sects and religions including Buddhism were introduced or already well-established by this time. In addition, books that examined ancient Chinese history made their appearance. One of the famous examples was Sima Qian (c. 14
-585 BC), who finished the classic
Shi Ji (The Historical Records) which detailed China's history from the earliest times to his own day. This set a standard for all subsequent Chinese historical writing. The quality of medical writings also improved as more medical texts were being written.
 |
| Confucius and his disciples, the sage's disciples played a decisive role in spreading his teachings. |
Due to the vast adoption of Confucian beliefs, most children took care of their parents when they were ill because this was considered the family members' responsibility. Consequently, many scholars and academics studied medical writings so they could perform the functions of a doctor should a doctor be unavailable. This led to an influx of philosophical thinking in the practice of Chinese medicine.

Searching for herbs |
Taoism and ImmortalityOne popular Taoist concept was that of longevity. Many emperors sought out herbs or elixirs that could make them immortal. Other religions such as Buddhism also aimed to discover the secrets of
Shangri-la by turning to
Taoism. For example, Emperor Lingdi (168
-189 AD) of the Han Dynasty invited Buddhist monks of another Taoist sect from India to his court in hopes that they would be able to provide him the elixir of immortality. These immortality elixirs were the origins of Chinese prescriptions.
Development of Medical System and EducationApprenticeships were a common means of educating new physicians in the Western Han Dynasties. These apprenticeships were mostly handed down through families because this insured a steady and reliable income. The prestige of the doctor was based on how many generations the family had been practicing medicine. In fact, one medical book from that period warned against taking medication from a physician if his family had been practicing medicine for less than three generations. The selection of apprentices was a stringent process. Even the
Huang Di Nei Jing (The Yellow Emperor's Classic of Internal Medicine) emphasized a careful selection of the apprentice since his success would bring the master fame. Other ways of becoming a doctor included studying prescriptions made by other doctors in a pharmacy or by self-study of medicine.
Examinations to recruit qualified physicians were introduced during the Han Dynasty. Emperor Yuan in 43 BC required all his attendant officials who were doctors to be tested. Interestingly, this examination was not necessarily based on medical knowledge, but rather the ability to be "simple in life, honest in dealings, polite in social intercourse, and good in conduct."
Basic medical service on a national level was also introduced during this dynasty. Physicians were divided into two groups. There were the imperial court physicians who attended to the emperor, and the physicians who attended to the army and the common people within the provinces of the empire.
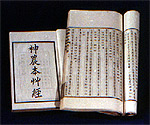 |
| Shennong Bencaojing (Classic of Herbal Medicine) |
Shennong Bencaojing (Classic of Herbal Medicine)
One of the most important medical books to come out of the Han Dynasty was the
Shennong Bencaojing (Classic of Herbal Medicine). The word bencao means "essential herb". While its attributed author is the
Fire Emperor discussed earlier, no one knows for sure who wrote it. What is known is that it was written between the 1st and 2nd century BC, and is considered to be the earliest complete Chinese pharmacopoeia reference.
This book lists a total of 365 Chinese medicines from which 252 were of plant origin, 67 from animals, and 46 from minerals. Each medicine was divided into one of three categories. The superior category included 120 medicines, which were considered to be non-toxic and contain invigorating effects to preserve vitality or prolong life. One of the most famous herbs in this category is ginseng (
Panax ginseng). The second category included average medicines of which 120 were listed. Medicines in this category were used to prevent illness and restore the individual's vitality. However, the medicines listed here containing herbs such as Chinese angelica (
Angelica sinensis) and ephedra (
mahuang) could sometimes be toxic and should be used carefully for certain ailments. The third category included 125 inferior medicines that were considered to be toxic with side effects, and were specifically used for therapeutic purposes to treat diseases. Croton (
Croton tiglium) is an example of an herb in this category which helps to relax the bowels, relieve edema (swelling) or eliminate
phlegm evils.
| Ginseng | Chinese angelica | Ephedra | Croton tiglium |
| Superior category | The second category | The third category |
Prominent Physicians of the Han DynastyDuring the Han Dynasty several prominent physicians emerged. Chunyu Yi (215
-167 BC) was the first doctor to keep "medical records" on the patients he treated. Guo Yu, who was the court physician of Emperor He, and Fu Weng were two doctors of the first century AD who were renowned for their skills in acupuncture and moxibustion.
 |
| A copy from Shanghan zabzabinglun (Discourse on Fevers and Miscellaneous Illnesses) |
Zhang Zhongjing also known as Zhang Ji (150
-219 AD) was considered to be a 'sage of medicine.' He penned a book called
Shanghan Zabinglun (Discourse on Fevers and Miscellaneous Illnesses), which dealt with the treatment of many febrile conditions. The book contains six parts, which correspond to the six pairs of meridians. It is significant because it discusses diagnosis and treatment methods based on an assessment of the symptoms of different pathological conditions. Later in the Song dynasty (960
-1279AD), his book was rewritten and divided into two books called
Shanghanlun (
Treatise on Febrile Diseases) and
Jinkui Yaolue (
Summary from the Golden Chest).

Hua Tuo |
Hua Tuo (141-208 AD) was a contemporary of Zhang Zhongjing. He traveled from town to town treating patients and learning from other doctor's practices. He is famous for his skill as a surgeon and his use of anesthesia. The anesthesia was given as a powder called mafeisan that was dissolved in a fermented drink before performing surgery. It has been suggested the powder may have been hemp since its uses were unknown at that time. Besides performing surgeries, Hua Tuo also recommended the use of physical exercises for his patients. He devised movements that were similar to the movements of five different animals. These were the tiger, deer, bear, monkey and bird. It is said that one of his disciples
Wu Pu lived to be 90-years-old due to these exercises. Another of Hua Tuo's disciples called
Fan A was a great acupuncturist. He devised methods to extend it use to the back and thorax. Unfortunately many of Hua Tuo's works have been lost, and surgery became unpopular because most Chinese beliefs and laws of the time did not look favorably on it.
Physical exercises - tiger, deer, bear, monkey and bird movements. |
Dong Feng was another well-known physician who practiced towards the end of the Han Dynasty during the reign of Emperor Xian.
The end of the Han DynastyIn 184 AD, the Yellow Turbans successfully broke up the Han Dynasty. The army generals held the real power and this led to the Three Kingdoms period of the 3rd century AD. One general called Cao Cao was especially militant. He has requested Hua Tuo to remain in his service after being treated for a migraine headache. After Hua Tuo refused, Cao Cao had him killed.
The Zhou or Chou Dynasty approx. 1100-221BCThis dynasty is divided into four periods: | * | Western Zhou | 1100-771 BC |
| * | Eastern Zhou | 700-256 BC |
| * | Spring and Autumn Period | 770-476 BC |
| * | Warring States Period | 476-221 BC |
* Western ZhouThe Western Zhou people migrated to the Shang region in 1111 BC, initially adopting the Shang's customs. However, over time people started to rebel against the ancient customs and beliefs. It was an age of political and social unrest with a breakdown in the morals of the people. Feudalistic states were constantly at war with one another.
Confucianism and Taoism Two important persons emerged from this period. One was Confucius (557-479 BC). Confucius  |
Confucius and Lao-zi |
was a social reformist and a teacher. He wanted to restore order in this time of chaos. His contemporary, Lao-zi (born in 590 BC), was the founder of Taoism. Taoism teachings were more philosophical whereas Confucianism teachings were more practical. Even today their philosophies are still important in the Chinese culture, and have helped shape the practice of Chinese medicine.* Eastern ZhouAn organized medical system developed during this period.Court Physicians
According to the book Rites of Zhou or Rites of Chou, which recorded the ceremonies or systems for that time, the Eastern Zhou period had an organized medical system in which court officials of the emperor were trained in a variety of medical specialties. For example, jiyi were physicians who cured internal illnesses, yangyi were physicians who cured external illnesses such as wounds, skin problems, broken bones and other traumatic injuries, and shiyi were physicians who dealt with dietary problems. The first official Chinese veterinarians also appeared during this time.
* Spring/Autumn Period
A number of physicians contributed a great deal of knowledge to TCM in this period. One notable physician was Bian Que. Bian Que's skills were based on the four fundamental examination procedures of Chinese medicine. He would observe his patient's tongue, nose, ears, face, eyes, mouth and throat, listen to his patient's speech, coughing, or other bodily vibrations, take a complete history of the patient's problem, and lastly he would feel the patient's pulse. Bian Que also believed illness was caused by the imbalance of yin and yang. Using these examination techniques, Bian Que was an expert in many fields of medicine including gynecology, pediatrics, ophthalmology, psychiatry and otorhinolaryngology (ENT).
* Warring States Period During the Warring States Period China's feudalistic government split into seven different states. It was around this time period that the yin/yang philosophyand the use of five elements to describe causes for illness, were further developed and their uses began to be taught in schools and written about in books.
Huang Di Nei Jing (The Yellow Emperor's Medicine Classic)
Although the Huang Di Nei Jing book's authorship is attributed to the Yellow Emperor, it was actually written  |
| Huang Di Nei Jing (The Yellow Emperor's Medicine Classic) |
by several authors over a long period of time. This book is further divided into two sections. The first is the Suwen (The Book of Plain Questions) that was written in the late Spring/Autumn and the Warring States periods. The second part is called the Lingshu (The Vital Axis) and was written sometime in the second century BC with revisions taking place up to the Han Dynasty (206BC- 25AD). This book is very significant because it was one of the earliest concise medical writings about Chinese medicine. Beyond medicine, this book also presents ethical, philosophical and religious considerations; the three themes that run through the book are the theory of Taoism, yin and yang, and the five elements.  |
The theory of Taoism, yin and yang, and the five elements are the main themes in the Huang Di Nei Jing |
In 1973 and 1974, excavation of the Mawangdui tombs revealed medical writing dating back to 168 BC One text called the Wushier Bingfang (The Fifty-two Prescriptions), detailed 52 ailments and 52 prescriptions, and was the earliest written reference of Chinese pharmacology. Despite the fact that these writings are the earliest known Chinese medical references, the Huang Di Nei Jing (The Yellow Emperor's Medicine Classic) still remains one of the most respected and studied texts on Chinese medicine. Even today scholars on Chinese medicine still refer to the wealth of knowledge in this book.The Shang People 1700-1100BC About the Shang
The Shang people, one of China's earliest ancestors, lived in the Yellow River basin of China. During this period, medical principles were very primitive in form, and based on myths and  |
oracle bones |
legends as well as experience. Inscriptions on oracle bones of buffalo and tortoise shells describe the use of wine and hot water as medicine, and the use of needles and bronze knives as surgical instruments. In addition, these oracles shed light on a number of diseases and illnesses. The Shang believed their existence was closely tied with the universe where they were located in the center with the heavens positioned above and the earth positioned below. The Shang also believed that the earth was "flat and divided into three concentric squares." The concept of the universe
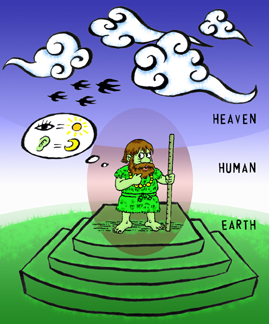 |
The concept of the universe |
was used to explain the laws of nature. Relationships were formed between the cosmos and humans. For example, the skin of the human body corresponded with the flat texture of the earth, the five internal organs corresponded to the five elements of wood, fire, water, earth, and metal, and the eyes and ears related to the sun and moon in the heavens. Antiquity 2200 BC  |
| Primitive clan |
During this period, different clans began to form, and survival was based on overcoming struggles with nature. As the early inhabitants hunted for food, they discovered that some foods could relieve illness while others were poisonous and could cause death. The discovery of fire was especially important because it allowed people to eat cooked food that was more easily digested.
 |
Discovery of fire |
 |
| Shamans(wu) |
At the same time, the generation of heat led to other findings. The earliest beginnings of using herbs, acupuncture, and moxibustion to cure disease were seen. While using hot stones to warm themselves, inhabitants realized that pressing them against certain parts of the body could help alleviate certain sicknesses. They also found that by using bone needles and pricking themselves in a particular spot could relieve pain in other areas of the body.
In addition, there were clan members who became specialists in these techniques, and were known as shamans (wu). The practice of medicine was very much integrated with magic to cure illness.
The Yellow Emperor and the Fire EmperorTwo well-known legends at the time were those of the
Yellow Emperor whose name was Huang Di, and the Fire Emperor who was bestowed the title
Shennong. Shennong has numerous meanings in Chinese such as "divine farmer", the "heavenly husbandman", and a more modern interpretation as a distinguished doctor. It is unclear whether these emperors actually existed but some historians date their existence back to 2500 to 2700BC.
 |
Shennong |
Both of these important figures are the attributed author's of two well-known books that have contributed significantly to Traditional Chinese Medicine. These are the
Huang Di Nei Jing(The Yellow Emperor's Medicine Classic) and the
Shennong Bencaojing (Classic of Herbal Medicine). In actuality these books were written much later in history. It was common in ancient time's for the Chinese authors to assign authorship of books to the great teachers or important persons who influenced them.
The Three Kingdoms Period 220 - 280 AD
| * | Wei | 220-265 AD |
| * | Shu Han | 221-263 AD |
| * | Wu | 222-280 AD |
(Carried over from Wu Kingdom)
| * | Western Jin | 265-316 AD |
| * | Eastern Jin | 317-420 AD |
| Southern Dynasty 420 - 589 AD |
(Carried over from Eastern Jin and ruled
Southern China)
| * | Song | 420-479 AD | | * | Qi | 679-502 AD | | * | Liang | 502-557 AD | | * | Chen | 557-589 AD |
| | Northern Dynasty 386 - 581 AD |
(Ruled Northern China)
| * | Northern Wei | 386-534 AD | | * | Eastern Wei | 534-550 AD | | * | Western Wei | 535-556 AD | | * | Northern Qi | 550-577 AD | | * | Northern Zhou | 557-581-AD |
|
About the Chinese Middle Ages
Renowned French, Chinese historian Jacques Gernet called the period from 200-581 AD, the Chinese Middle Ages. The Han Dynasty ended with the military taking over China and splitting the country into three kingdoms.  |
| The empire of the Three kingdoms (250 A.D.) |
During this time, the Northern Chinese were considered to be more militant and less sophisticated than their Southern counterparts. At the same time, Buddhism was rapidly spreading throughout all parts of China. The Northern Wei especially welcomed the religion's presence because it was seen as a way to consolidate power. Buddhism also led to the influx of Indian culture into China.
As a result, knowledge concerning mathematics, astronomy and medicine flourished during this period. Many monks had medical knowledge because it was a necessity when making long pilgrimages to be able to administer medical care when no doctors were available.
Development of Physician EducationDuring this time, medical education was elevated to a higher standard. In 443 AD, Qin Cheng-zu, an imperial medical officer, petitioned Emperor Wen of the Song Kingdom to appoint physicians to teach medical students. It was the first time the government assigned teachers to educate students on Chinese medicine. Although the Imperial Academy was established in 124 BC, it mainly focused on teaching subjects such as literature, philosophy and administration. Little emphasis was placed on medicine. However, by 493 AD, the Imperial Academy had expanded to include lectureships and chairs for teaching Chinese medicine.Acupuncture and MoxabustionAcupuncture, known as zhenjiu in Chinese, was widely accepted by the Chinese population. Its use may have originated out of the Chinese fascination of relieving referred pain, defined as pain that manifests in one part of the body but originating from somewhere else. Many of the physicians mentioned previously such as Qin Yueren, Zhang Zhongjing, Hua Tuo, and Fan A used this therapy when treating patients. The Lingshu (The Vital Axis), a book from the Huang Di Nei Jing (The Yellow Emperor's Classic of Internal Medicine) has a whole section dedicated to the use of acupuncture. 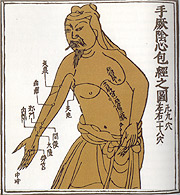 |
| Meridian with acupuncture points |
| Zhenjiu Jiayijing (The ABC of Acupuncture and Moxibustion) |
The man who wrote what is considered the bible of accupuncture and moxibustion was Huangfu Mi (215-282 AD). His biggest contribution was a book called Zhenjiu Jiayijing (The ABC of Acupuncture and Moxibustion), which is considered to be the earliest complete reference guide to acupuncture and moxibustion. This book starts by discussing TCM concepts involving anatomy, and physiology and progresses to describing the theory of meridians. In addition, it outlines the location of the acupuncture points, discusses the techniques used to manipulate the needles, and describes the clinical applications and therapeutic benefits of both acupuncture and moxibustion.
Meridian and Pulse StudyBy now the concept of blood and circulation was fully entrenched in the practice of Chinese medicine. It was thought that there were two separate systems of circulation within the body, each with a different fluid flowing though it. Blood was known to pump from the heart and into vessels throughout the body. Qi was considered a form of energy that pumped from the lungs, and circulated throughout the body on invisible tracts called meridians or channels.
| Wang Shuhe and the Maijing (Pulse Classic or Manual on the Pulses) |

Wang shuhe, the Promoter of Pulsing |
Wang Shuhe (265-317 AD) wrote the Maijing (Pulse Classic or Manual on the Pulses), which was a compilation of all the knowledge on pulse diagnosis up to this point in history. In Chinese medicine feeling the pulse is perhaps the most important examination technique used when diagnosing a patient because how a pulse feels indicates different illnesses. In this book, 24 different kinds of pulses were identified. Chinese Prescriptions
Taoist doing experiments |
Alchemists can be considered the first pharmacists. Their popularity arose out of the Taoists quests for longevity. In their search for the magic elixir of life, alchemists would experiment with different methods of combining chemicals and minerals to create new medicines or tonics. Ge Hong (281-341AD) 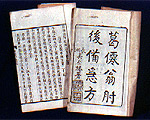 |
| Zhouhou Jiuzufang (Emergency Prescriptions) |
a famous alchemist and physician at that time. His greatest achievement was his book Zhouhou Beijifang or Zhouhou Jiuzufang (Emergency Prescriptions or Handbook of Medicine for Emergencies) which was considered to be a "how to" guide for medical emergencies. It was concerned with practical approaches to medical problems and included prevention strategies such as the use of quarantine for contagious diseases. In his book, he proposed cures that were quick, cheap, and easily accessible. Some are still used today. For example, ephedra sinica is used in the treatment of asthma and dichroa febrifuga is used to treat malaria. Illnesses discussed in this book included typhoid, dysentery, malaria, smallpox, leprosy and cholera, which were common during those times. Materia Medica Another important figure in the development of Chinese medicine was Tao Honjing (456-536 AD), who was especially renowned for his commentaries on the Shennong Bencaojing (Classic of Herbal Medicine). He increased the number of listed herbal medicines in the Shennong Bencaojing (Classic of Herbal Medicine) from 365 to 730, and furthered the information on the herbs' nature, location, and time of harvesting. The new book was entitled Shennong Bencaojing Jizhu (Annotations to the Classic of Herbal Medicine). It dominated the pharmaceutical literature until the middle of the 7th century A.D. He also completed Ge Hong's Zhouhou Beijifang (Emergency Prescriptions), which was re-titled Zhouhou Baiyi Fang (101 Emergency Prescriptions). 
Wall picture of Buddhist caves - people used water and fire to prevent contagious diseases |
These prescriptions and those of other alchemists and Chinese doctors were often circulated using handwritten copies. Sometimes they would also be carved into the stone caves that served as Buddhist sanctuaries. One example is the Buddhist caves of Longmen (also called Dragon's Gate located south of Loyang in Henan province). There you can find approximately 100 prescriptions carved into the walls near the end of the 6th century AD Ge Hong's use of dichroa febrifuga for the treatment of malaria is an example of one such prescription carved at this location.
Other Important Medical Contributions
Other important Chinese medical works of this time are Lei Xiao's (born in 15 AD) Leigong Baozhilun (Treatise on the Preparation of Lei Gong's Remedies) and Liu Juanzi Guifang, the earliest known treatise on Chinese surgery. Lei Gong Baozhilun (Treatise on the Preparation of Lei Gong's Remedies) focused on the vegetable-based medicines unlike Ge Hong's work that focused on chemical remedies to cure illnesses. In addition, this book outlines the various ways of preparing these medicines such as cooking them over an open fire , steaming or boiling them . The later book, Liu Juanzi Guifang, provides a wealth of information on the experiences gained up to the fifth century in the treatment of wounds caused by metal instruments and of ailments affecting the skin such as boils, anthrax and abscesses. The use of mercurial ointment is mentioned for curing certain skin conditions.The Sui Dynasty 581-618 AD
About the Sui Dynasty During this time, there was a desire to reunite China again and restore the country to the former glory that the Han Dynasty (206BC - 220AD) enjoyed. A general from the Northern Zhou Dynasty was successful in overthrowing the last Southern Dynasty (Chen) in 581 AD. This general adopted the reign title of "Sui Wendi," or emperor Wen, thus establishing the Sui Dynasty. However, this dynasty was short lived due to the problems stemming from peasant revolts and the burden of a military campaign launched against Korea. Sui Wendi's successor, Sui Yangdi was overthrown and the Tang Dynasty was established in 618 AD.
Chao Yuangfang
Approx. 610A.D. |
ChaoYuangfang (c. 610 AD)
Chao Yuangfang was a
taiyi, which was the title for the emperor's physician. He is most famous for his book entitled
Zhubing Yuanhoulun (Treatise on the Causes and Symptoms of Diseases). This book is comprised of 50 volumes and describes 1,700 syndromes. It is significant because it is the earliest record in China that categorizes the causes, symptoms and pathology of certain diseases in a systematical manner. It touches on subjects concerning internal medicine, surgery, pediatrics, gynecology, dermatology, ophthalmology, and
ENT.
The Tang Dynasty 618-907 ADAbout the Tang Dynasty
The Tang Dynasty was founded by the Li family. Li Yuan, the first emperor of the Tang Dynasty, reigned under the name Tang Gaozu (618-626 AD) followed by his son Li Shimin who reigned under the name Tang Taizong (626-649 AD). The early Tang Dynasty expanded China making it the most powerful Asian country. During this time, Buddhism was at its peak and Chinese poetry flourished.
 |
| Tang Empire (618-907 AD) |
The Imperial Academy
In 624 AD, another Imperial Medical Academy was founded. This government run academy graduated doctors for the purpose of serving the emperor, his family, and the nobles. It was a large institution divided into two areas: medicine and pharmacy.
| A Medical Charm: Chinese people believed it had magical power for healing. |
Medicine: Those students who studied medicine were required to take general subjects that focused on classics such as the
Huang Di Nei Jing (The Yellow Emperor's Classic of Internal Medicine), Shennong Bencaojing (Classic of Herbal Medicine), Maijing (Pulse Classic or Manual on the Pulses), and Zhenjiu Jiayijing (The ABC of Acupuncture and Moxibustion). Clinical subjects studied included areas such as internal medicine, pediatrics, surgery,
ENT,
cupping, acupuncture, massage and charms and incantations. This last subject (charms and incantations) arose out of the influences of Taoism and Buddhism on Chinese culture, and is significant because it reflected the importance that spiritualism played in the holistic healing process.
Pharmacy: Those students studying pharmacy helped maintain the Imperial Academy's herb garden and learned how to plant and process herbs. Upon graduation, they were made herb gardeners.

Examination in ancient times |
Examination Process: One of the most important aspects of this school was the examination process that all students were required to go through. There were seasonal and yearly examinations of all the subjects studied. If a student failed the final examination required for graduation, he was dismissed from the academy. Doctors were promoted based on their treatment success rate. The implementation of exams to qualify doctors may have been a catalyst for Western countries to adopt their own examination process. In 931 AD, the Arabs began requiring qualifying examinations for medical practitioners, and in 1140 AD
Roger of Sicily passed laws requiring state examinations for doctors in Italy.
By 629 AD, just five years after the Imperial Medical Academy was established, emperor Tai zong established local medical schools to educate the doctors in the outlying provinces. By 713 AD, China's local government was assigning assistant teachers to these schools, and by 723 AD the local government's power expanded so that they had the authority to appoint medical doctors to serve the lay public. As a result, apprenticeships were now not the only means for local doctors to learn medicine as formalized medical education became popular.
The First Official Pharmacopeia  |
Xinxiu Bancao (Newly Revised Materia Medica) - The First Official Pharmacipeia |
The previously mentioned
Shennong Bencaojing (Classic of Herbal Medicine) written in approximately the 1st and 2nd century BC is the earliest pharmacopoeia reference. It was later revised by Tao Honjing (456-536 AD) and renamed the
Shennong Bencaojing Jizhu (Annotations to the Classic of Herbal Medicine). While both of these works are very important, the authors wrote these books of their own accord because of their passion for medicine. It was not until the Tang Dynasty that the first official pharmacopoeia was mandated by the government. A physician named Su Jing, along with approximately 20 other of his compatriots wrote the
Xinxiu Bencao (Newly Revised Materia Medica) between 657-659 AD, which was the first official pharmacopoeia in China and in the world. Western cultures would not have
official pharmacopoeias until several centuries later.
Foreign Influences on Chinese Medicine Development

The Buddhist pilgrim to India - shown carrying back the scriptures to China |
Due to China's expansion and improvement in communication and transportation systems, Chinese medicine was introduced into foreign cultures. In return, these foreign cultures contributed to the advancement of Chinese medicine by expanding its knowledge base. Chinese doctors were sent to countries such as Korea, Japan, India and Vietnam, and many of the previously mentioned Chinese medical texts were exported and translated into these countries' languages. From Korea, herbs such as ginseng , giant Typhomium tuber (
bai fuzi), Korean pine and others were introduced into China. From Vietnam came vanilla grass, sappan wood, and cloves. Due to the popularity of Buddhism and the frequent pilgrimages of religious monks, a natural exchange of information occurred between China and India. Many Indian medical books were translated into Chinese, and Indian doctors were known to practice in China. Advancements in ophthalmology were in part attributed to Indian experience. In return, herbs such as ephedra, ginseng, and angelica were brought from China to India.
Chinese medicine also influenced the Arab world as Arab merchants made their way into China. The Arabs brought back alchemy and
Pulsology techniques as well as herbs such as rhubarb and cinnamon while new substances such as incense, myrrh, and fenugreek (
Trigonella foenum-graecum) were given to China. The fig (
Ficus carica), which is known for its laxative properties and is still used in Chinese medicine today, came from Persia. Tibetan medicine also benefited greatly from both Chinese and Indian influences.

Sun Simiao (581-682 A.D.) - King of Prescriptions |
SunSimiao (581-682 AD)
Sun Simao is one of the most influential physicians in the history of Chinese medicine, and is distinguished by his application of medicine and his adherence to an ethical code. His interest in medicine came from his own fragile health whereby he treated himself as his first patient. His mastery of medicine, Buddhism, Confucianism, and Taoism made Emperor Wen of the Sui Dynasty, and Emperors Tai-zong and Gao-zu of the Tang Dynasty seek him out as an imperial physician. However, Sun Simiao declined these posts and devoted his life to being a physician who served the common people. He believed the best way to care for a patient was to prevent an illness before it occurred. The worst care was to treat an illness that had already occurred because it meant that he was unable to keep his patient healthy.
Sun Simiao's best known works are
Qianjin Yaofang (Prescriptions Worth a Thousand Gold for Emergencies or Precious Prescriptions for Emergencies) and the
Qianjin Yifang (A Supplement to the Essential Prescriptions Worth a Thousand Gold or Supplement to Precious Prescriptions). The first book is comprised of 30 volumes and lists 5,300 prescriptions. The second book is also made up of 30 volumes and lists 2,571 prescriptions. Sun Simiao's observations about diseases and his prescribed treatments are noteworthy even today. For example, he knew cholera and diarrhea were caused by what people ate and drank and not by "evil spirits" as was commonly thought. He correctly identified tuberculosis as a lung disease, which was a new concept of this time. After successfully treating 600 cases of leprosy, he is considered the earliest expert on this disease in China.
Sun Simiao is also renowned for his identification and treatment of deficiency disorders. Even though he was not exactly sure of the cause of goiter (hypothyroidism caused by lack of iodine), he knew it occurred in people who lived in certain mountainous regions and drank unsanitary water. He prescribed medicine from the thyroid glands of deer and sheep because they are high in iodine content. Nyctalopia, which is night blindness caused by lack of vitamin A, was successfully treated with pig, calf and sheep livers that contain large amounts of this vitamin. He is the first person in the medical history to document the diagnosis, treatment, and prevention of Beriberi, a deficiency disease caused by lack of vitamin B1. For this, he prescribed combinations of herbs that were high in Vitamin B1.
Qi Gong |
The elderly also benefited from Sun Simiao because he was a strong advocate for maintaining health throughout a person's life. He thought life could be prolonged with measures such as performing daily breathing exercises (qi gong), regular physical exercise, and massage therapy. He advised against excessive drinking, eating raw meat, and spitting in public. He also believed diet therapy should be tried before resorting to medicine.
Other advances made by Sun Simiao were in the areas of acupuncture, moxibustion and pharmacy. He thought moxibustion should be performed prior to acupuncture, and he was successful in determining essential acupuncture points. Sun Simiao also combined acupuncture with drug therapy, and stressed using the
a- shi point, which is still used by acupuncturists today. His knowledge of herbs was vast, and he insisted on harvesting them in the proper season and processing them correctly. The nickname "king of pharmacology" or 'king of prescriptions" was given to him because he was especially knowledgeable in preparation of medicinal herbs.
Five Dynasties 907 - 960 AD | * | | Later Liang | 907-923 AD |
| * | | Later Tang | 923-936 AD |
| * | | Later Jin | 936-946 AD |
| * | | Later Han | 947-950 AD |
| * | | Later Zhou | 950-960 AD |
With the collapse of the Tang Dynasty, China was ruled by a series of short-lived dynasties originating from Kaifeng. As a result, the country was divided into independent states.
 |
| Territories of China in 930AD |
The Liao Dynasty 916 - 1125 AD
The Liao was a powerful dynasty in the North established by the Khitan people. The Song Dynasty which coexisted with the Liao Dynasty was required to pay huge sums of money to them in order to maintain peaceful relations and prevent invasion.
The Northern and Southern Song Dynasties 960-1279 AD
| * | | Northern Song | 960-1127 AD |
| * | | Southern Song | 1127-1279 AD |
About the Song DynastiesZhao Guangyin reunified China and founded the Song Dynasty in 960 AD. The empire was continually threatened on all sides by invasion from barbarians. Besides problems in the north with the Liao Dynasty, the Song also had to contend with the Tibetans and the Tanguts tribe to the west. Eventually, the threat of invasion became a reality and the Jurchen (an isolated clan originating from the Tanguts tribe) established the Jin Dynasty in the north in 1127 AD. This forced the Song south into Hangzhou where they would remain until the late thirteenth century when the Mongols invaded China.
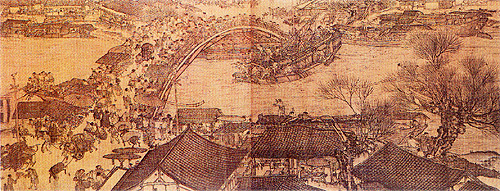
 |  |
| Northern Song 960-1127 AD. | Southern Song 1127-1279 AD. |

A busy market scene in the Song Dynasty. |
Fueled by economic growth from agriculture, an urban bourgeois class emerged. The bourgeois indulged in comforts of daily life and lived extravagantly. Marine trade expanded significantly due to both an increase in commercial trade and the growing difficulty of making overland trips because of the barbarian control of trade routes. Confucianism saw resurgence in this period and was later renamed neo-Confucianism by philosophers. Other new philosophies evolved and these were also applied to medicine. The period was further buffeted by a series of reforms and counter-reforms. The "new laws" of the dynasty introduced by Wang Anshi
(1021-1086 AD), a prime minister in Northern Song, are held to have constituted radical political changes in China. The changes facilitated medical reorganization and enabled new healthcare systems or facilities to be set up, these included government dispensaries, hospitals, and charitable institutions.
Publishing Boom of Chinese Medicine Texts
 |
| Woodblock printing |
The use of woodblock printing, although existent since the Tang Dynasty in 868 AD, was further improved by Bi Sheng in 1040 AD with the invention of
movable type. This had a significant impact on Chinese medicine and science in general as it enabled important texts to be more easily published and readily disseminated.
During this period, a state institution known as the "Bureau for the Re-editing of Medical Books," was created in order to "collect, collate and verify all medical texts bequeathed by 1,000 years of history." This bureau published several of the established classics and many books were rewritten or revised under new titles. Therefore many classics like
Huang Di Nei Jing (The Yellow Emperor's Classic of Internal Medicine),
Shennong Bencaojing (Classic of Herbal Medicine),
Maijing (Pulse Classic or Manual on the Pulses), and
Zhenjiu Jiayijing (The ABC of Acupuncture and Moxibustion) etc, have been handed down after being checked and printed. The bureau also produced commentaries on classics such as
Huang Di Nei Jing (The Yellow Emperor's Classic of Internal Medicine) and Zhang Zhongjing's
Shanghanlun (Treatise on Febrile Diseases).
In addition, many medical texts were published under government supervision or individually. Campaigns were launched by the Song government for gathering information from the public and for the periodic compilation of medical texts. A great deal of original material in the form of pharmacopoeias were written.
| * | Important pharmacopoeial texts are ...... |
Besides pharmacopoeias, many prescription books were also published. The first one, entitled
Taiping Shenghuifang (Prescriptions from the Pharmacy of Harmonious Assistance), was commissioned by the government and written by Wang Huaiyin at the end of the tenth century. It lists a total of 16,834 prescriptions and gives details of the prescription, drugs used, syndromes and pathology.
| * | Other notable prescription texts written during this time are....... |
The number and variety of such works testify to the flourishing state of Chinese medicine at the time.
A Chinese peasant being treated by a village doctor with moxibustion. |
Medical EducationDuring the Song Dynasty, medical administrative duties and medical education were separated. The government's "Board of Medical Officers" was in charge of overseeing the practice of medicine and the delivery of medical care.
Wang Anshi an important political figure of the eleventh century initiated sweeping reforms that included developing a more perfect examination system and curriculum in medicine. As a result of his reforms, the Imperial Medical Bureau (taiyiju), which was in charge of medical education, expanded to become the Imperial Medical College. Soon after, a number of medical schools were founded in different cities or towns in China and this extended medical knowledge to a more popular level
.Examinations for medical students were also launched during this period and were set up along similar lines to those for civil servants. Students were promoted to the next level based on their scholastic records and their treatment success rate. The Imperial Medical College was further divided into nine departments:
| 1. | Internal medicine | 6. | Dermatology and orthopedics | | 2. | Obstetrics | 7. | Acupuncture and moxibustion | | 3. | Pediatrics | 8. | Trauma and incantations | | 4. | Ophthalmology | 9. | Wind diseases (treating diseases such as stroke) | | 5. | Ear, nose, throat and dental | | |
|

Wang Weiyi
(987-1067A.D.) |
Besides studying the
earlier classics of the Tang Dynasty, medical students would have newly created curricula, such as the "three causes" (
sanyin) theory by Chen Yan (see
A new teaching section), added by the end of the twelfth century. Students also became more familiar with
anatomy as illustrations drawn by the physician/poet Yang Jie (1068-1140 AD) from autopsies of executed prisoners became available.
 |
| Bronze model of acupuncture points |
Another advancement in medical education was the casting of two life-size male bronze statues by Wang Weiyi (987-1067 AD), an officer of the medical board, appointed to summarize the acupuncture classics for teaching acupuncture. These statues had 657 acupuncture points drilled into them which were filled with water and covered with wax. When a student needled the acupuncture point correctly, water would leak out. To complement the statues, Wang Weiyi compiled a book called
Tongren Shuxue Zhen Jiu Tujing (Illustrated Manual of the Bronze Man Showing Acupuncture and Moxibustion Points). This work was considered so important that it was carved on two stone steles and these were erected in Kaifeng, the capital of the Northern Song Dynasty, for public use. The bronze statues would contribute significantly to the future education of acupuncturists.
A New Teaching: Theory on the Three Causes
As mentioned, a new approach to etiology was first propounded by the twelfth century physician, Chen Yan. His work
Sanyin Jiyi Bingzheng (
A Treatise on Pathology) stated that there are three types of pathogenic agents(
sanyin): endogenous, exogenous, and those that are neither one nor the other. These influences lead to an imbalance between the yin and yang in the body, between the vital energy (
qi) and the blood, or impair functions of organs and meridians, all of which give rise to illness. This principle has been applied by traditional Chinese medicine physicians until today.
| * | The classification of pathogenic agents (sanyin) are...... |
Poison victim |
Medical Advances in Forensic Medicine
Xiyuan Jilu or Xiyuanlu (
Washing Away the Wrongs) was written by
Song Ci in 1247 AD. The book details how to perform autopsies and lists observations about physiology, histology, pathology, pharmacology, and toxicology. According to this book, someone who has been fatally poisoned will present with a green or purplish complexion, the eyes and mouth will be wide open, the nails on the hands and feet will be blue, and blood may trickle from the eyes, mouth, ears, and nose. To confirm that poisoning has taken place, a silver needle that has been scrubbed in soapy water should be stuck into the victim's mouth. If the needle turns a blackish color that cannot be washed off, then poisoning is confirmed. This book helped establish the beginning of forensic medicine in China and would go on to be an important medical work that was translated into at least five different European languages.
 |
| Children and woman of the Song Dynasty |
Pediatricians and Gynecologists During the Song dynasty, the interest in medicine shown by the Song authorities led not only to official support for the publication of general medical works but also to a new surge in medical studies. Pediatrics and gynecology became a specialized and independent branch of medicine, and obtained significant results.
The most important figure in pediatrics was
Qian Yi (1035-1117 AD). His work was recorded by his disciple Yan Xiaozhong in the
Xiao'er Yaozheng Zhijue (The Appropriate Way of Recognizing and Treating Infant Maladies.) Moreover, Qian Yi contributed to a better understanding of eruptive fevers, such as smallpox, chickenpox, and measles, in terms both of symptoms and therapies. It dealt entirely with infant medicine, considered under its physiological, pathological and therapeutic aspects.
| * | Other famous pediatricians or texts of the Song dynasty include...... |
The Song Dynasty had developed public welfare in the urban areas with the opening of dispensaries, hospitals, and orphanages. Urbanization obliged the authorities to make special arrangement for public hygiene. In some places during the Southern Song period, road-sweepers and night-soil collectors were a daily presence. Evidence also points to the use of spittoons. Preventive measures against contagious diseases were set up by the government. The common occurrence of smallpox at that time, the cause of a very high infant mortality rate, stimulated studies in the disease.
|
| * | Studies in smallpox during the Song include...... |
The fields of gynecology and obstetrics had begun to take on the hallmarks of an independent branch of medicine. Chen Ziming (c. 1190-1270 AD) produced a work, Furen Daquan Liangfnag (Collection of Gynecology Treatises), which specifically dealt with various gynecological problems associated with menstruation, pregnancy, and childbirth. A whole chapter of his book is devoted to cases of dystocia (difficult childbirth) and several examples are described: shoulder-, face-, and breech-delivery.
|
| 
Smallpox in children |
|
| * | Other famous gynecologists or texts of the Song Dynasty include...... |
Foreign InfluencesDue to the remarkable expansion in marine trade, exchange of information between East and West reached a peak at this time. There are records that Arabian merchants shipped over 60 different items of materia medica to European, Asian, and African countries. Included amongst these were cinnabar, ginseng, monkshood, pepper, tuckahoe (Indian bread), and bezoar.
Bezoar was regarded as the most valuable and was held important at that time for the prevention of epidemics. The relationship that China enjoyed between the tenth and twelfth centuries with Korea, Japan, South-east Asia, and the Arab world facilitated mutual exchanges in the fields of medicine and pharmacy. Among the items of tribute offered by various states to the Chinese emperor, it is common to find animal, vegetable and mineral products that were to be used in the manufacture of medicine. Such were rhinoceros horn, ivory, rose-water, pearls, coral, and melon. In return, many medical classics or physicians were sent to these states and this greatly influenced their medical development. Nowadays, copies of many ancient classics which have been lost in China can still be found elsewhere in the world.
 |
| Port in the Song Dynasty |
The Jin-Yuan Period 1115 - 1368 AD
* The Jin Dynasty 1115
-1234 AD
* The Yuan Dynasty 1279
-1368 AD
About Jin and Yuan 
Mongol Horsemen Hunting |
The Jin and the Yuan were neighboring nomadic non-Chinese tribes who lived in the north-east of the empire during the Song Dynasty before they developed their own powerful kingdoms. The Jin Dynasty was founded by a Tanguts tribe in 1115 and conquered the northern part of China in 1126. This situation prevailed for more than one-hundred years until a strong Mongol army overthrew the Jin in 1234. The Mongols then defeated the Southern Song in 1279, taking over the whole region to found the vast Yuan Empire. During this time, China was totally under foreign rule and historians refer to the period as the Jin-Yuan.
In the 13th century, the Mongols rose to power under the leadership of
Genghis Khan. Under his successor, his third son Ogodei (1227-41), as Great Khan, led Mongol armies into Europe as far as Poland and Hungary. In 1279, it was the grandson of Genghis Khan, Kublai Khan, who founded the Mongol Dynasty, giving it the Chinese name of Yuan, and established his capital in Beijing. Under Mongol rule, the kingdom proved disjointed and divided. There were nine rulers who held the throne during this short period and as a result power was weakened. Chinese officials were once again able to gain a foothold when in 1368 a rebel Chinese group, the Red Turbans, ended the Yuan Dynasty.
Map of Mongol Empire |
The culture, art and lifestyle of the country during the period remained basically the same as it had during the Song Dynasty, but the prosperity of the previous dynasty began to fade. The Jins wiped out some of the Song's most talented artists. Creativity and inventiveness began to disappear. Under Mongol rule, a whole new set of rules and customs were created. The Mongols prohibited marriage between different ethnic groups and heavily taxed the peasants. In response to what they considered unjust and unfair treatment, a number of religious societies, including Buddhist-based associations, revolted.
On the positive side, Mongol rulers imposed a strictly regulated system of medical practice and banned the use of certain toxic drugs. In 1268, for example, the sale of aconite and arsenic was forbidden. The Mongols also helped open trade in the region known today as the Middle East. One of the best-known explorers of the time was
MarcoPolo. The Italian-born explorer was the first European to really journey through the Asian continent.
Prominent physiciansDuring this period, several schools of thought evolved attributing disease to different factors, and advocating contrasting approaches to treatment. This was in addition to the Mongol physicians who held their own set of beliefs. Nevertheless, a number of physicians living at this time made a significant contribution to medical development.
Liu Wansu
(1120-1200 AD) |
Master Hejian (Liu Wansu) Liu Wansu (1120-1200), or Master Hejian as his students called him, is credited with founding the Hejian School. A native of Hebei province, he three times turned down an offer from the Jin emperor to practice medicine for the palace and chose instead to practice medicine for the people. He played a significant role in the development of Chinese medicine and is famous for writing a number of works based on the medical classic the
Suwen (The Book of Plain Questions).
Liu Wansu's belief centered on the theory of the
five movements (yun) and six influences (qi). He placed particular importance on the elements of fire and heat, and tended to prescribe herbs that have cold properties to treat disease arising from these influences.This is also referred to as the "
School of cooling" for the reason. Examples of his frequently prescribed herbs are cassia twig,rehmannia root, ephedra and mint.
Zhang Congzheng
(1150 - 1228 AD) |
Six Doors and Three Methods (Zhang Congzheng)Zhang Congzheng (1150-1228) had an innovative approach to medical treatment and insisted that the medicines of yesterday could not combat present-day illnesses. He was a military physician and wrote a book called
Rumen Shiqin (Therapies for Scholars) based on his observations and research. However, he is best known for his theory of the "
six doors and three methods." The six doors are the six influences (wind, summer heat, dampness, fire, dryness and cold) that Liu Wansu observed, and the three methods refer to therapeutic regimens used to induce
sweating, vomiting and purging, that Zhang resorted to frequently. He thought that evil influences were derived from
the heavens, the earth and man's behavior (e.g. what he ate). In order to effect a cure, the evil influences had to be expelled.
Master of the Yishui School (Zhang Yuansu)Zhang Yuansu (1151-1234) was the founder of the Yishui School, named after his native district in Hebei province. According to his book
Yixue Qiyuan (Explanation of Medicine) published in 1186, "the prescriptions of the past were not appropriate for the illnesses of today."
However, Zhang created a unique mosaic of his own practices and beliefs based on the teachings of his predecessors in medical classics such as the
Huangdi Neijing (The Yellow Emperor's Classic of Internal Medicine), the Shanghanlun (Treatise on Febrile Diseases) and the
Zongzangjing . Zhang Yuansu was known for his idea that medicine has specific effects on particular meridians. He thought illness occurred when there was an imbalance of
zang and fu organs. By understanding the pathological conditions of the organs, a diagnosis could be made and appropriate therapy could be chosen.
Li Gao
(1180 - 1251 AD) |
The Old Gentleman of the Eastern Wall (Li Gao)Li Gao (1180-1251) had been fascinated by medicine since childhood. Li, who came from a wealthy family, is known for his concern about how lifestyle affects the body's organs. In his most important work,
Piweilun (Treatise on the Spleen and Stomach), he stated that if the spleen and the stomach were injured by an inappropriate lifestyle, vitality would decline and illness would result from an imbalance of qi in these organs. He was a strong believer that a person's emotions, including anger, joy, sadness and grief, could heavily influence the qi, and that illness was caused by a society marred by poverty, war and oppression. He was a proponent of the use of several tonics and especially recommended ginseng.
Zhu Zhenheng
(1281 - 1358 AD) |
Minister of Fire (Zhu Zhenheng) From Zhejing province, Zhu Zhenheng (1281-1358) was also known as Master Danxi. He undertook a systematic study of medicine and his work,
Gezhi Yulun (Theories of In -depth Research), studies the theory of internal fire or heat during physiological and pathological change in the body. Minister-fire is a kind of yang energy that is a vital force necessary for the body to function. It mainly exists in the liver and kidneys. It cooperates with the second fire, "master-fire" or heart-fire, to promote the function of the organs. In illness, Zhu Zhenheng thought that the body's yang was usually in excess causing yin to become deficient. As a result, "fire" in the body, which is normally produced by movement, was increased during the course of disease and was thought to be due to disharmony of the minister-fire. As a yang excess was thought to be harmful because it consumes yin, nourishing the yin and quenching the fire were the chief measures of treatment. Zhu Zhenheng strongly recommended appropriate diet and sexual activities in order to preserve the yin. This theory of "minister fire" is still used today in TCM.
Acupuncture and Moxibustion
Location of Acupoint Jiuwei |
In the Jin-Yuan period, acupuncture and moxibustion were used extensively and various acupuncture points and their corresponding therapeutic virtues were validated further. Procedures in applying acupuncture and moxibustion to these points had been developed differently over the centuries.
Four Books of Acupuncture and Moxibustion (Zhenjiu Sishu) published by Dou Guifang in 1331 compiled important works written during the Song and Jin Dynasties on acupuncture. For example, a point known as jiuwei (see picture) mentioned in
Huangdi Mingdang Jiujing (one of the four books) was used in treatment of palpitations and epilepsy, a point whose use is endorsed by contemporary acupuncture practice for similar indications. It was not only the Chinese who made discoveries and developed new theories regarding acupuncture and moxibustion. The Mongols also contributed to medical knowledge. Therapeutic methods like Mongolian moxibustion and blood-letting were very popular at that time.
A copy from Shiyi Dexiaofang
(Efficacious Remedies of the Physicians) |
Bone Setting and Traumatic SurgeryNomadic Mongols were involved in continuous military activity and this further facilitated the development of external medicine. During the Yuan Dynasty, Qi Dezhi and his work
Waike Jingyi (The Essentials of External Medicine), dating from 1335 AD, represented the achievement of the time. Although the book outlines various therapeutic methods using minor surgery, it lists remedies making use of decoctions, pills, powders and ointments and is more a treatise on dermatology than surgery. He believed that disorders of the skin were a consequence of imbalance in yin and yang. Phytotherapy (use of herbs) was an integral part of Qi Dezhi's approach.
Wei Yilin (c. 1277-1347) a contemporary of Qi Dezhi specialized in orthopedics. His book
Shiyi Dexiaofang (Efficacious Remedies of the Physicians) is a testimony to Wei's skills in setting fractures and in treating dislocations of the shoulder, hips and knee. He also made occasional use of anesthetic drugs and pioneered the suspension method for joint reduction. It was not until 1927 that this was introduced into Western medicine by the British doctor, Davis.
Dogmeat from Yinshan Zhengyao (Important Principles of Food and Drink) |
Eating for Health the Chinese Way
Hu Sihui, a Mongol, is credited for being a distinguished dietician. He wrote
Yinshan Zhengyao (Important Principles of Food and Drink) in 1330 and was a proponent of a balanced diet. He especially focused on the importance of moderation and championed the eating in moderation rule. In addition, Hu's book offered a list of 230 cereals, meat, fish, shellfish, fruits and vegetables with a description of their nutritional benefits. For example, Hu said that eating too many apples caused distension and too many oranges could harm the liver; that dog meat was salty, not too overpowering, non-toxic and calmed the zang organs; and that grapes sustain energy and strengthen character.
Other Important Works
Other practitioners during the Jin-Yuan period included Ge Keijiu (1305-52) who wrote a treatise,
the Shiyao Shenshu (1348), on tuberculosis and Zeng Shirong whose book
Houyou Xinshu (1294) expanded the study of pediatrics from the Song Dynasty.
Ming Dynasty 1368 - 1644 ADAbout the Ming
 |
| Map of Ming Dynasty |

Emperor Hongwu |
The founder of the Ming dynasty was Zhu Yuanzhang, better known as Hongwu. Hongwu was a Han Chinese peasant and former Buddhist monk turned rebel army leader. He led the defeat of the Mongols in 1368 AD Extensive political and agricultural reforms were undertaken by the early Ming resulting in a period that was both rich and fruitful in terms of economy, art and culture. This was especially so under the reign of the second Emperor Yongle, 1403-24. Under Emperor Yongle's leadership China flourished. This was a period of many firsts. The Forbidden City was constructed, dictionaries such as the Yongle Dadian (Great Dictionary of the Yongle Reign) were written and explorers such as Zheng He traveled the world for new ideas. Famous literary works such as the Xiyouji (Journey to the West) and Jin Ping Mei (The Golden Lotus) were written during this time. Despite such progress, the dynasty became increasingly dictatorial and the Ming reign was to be short-lived. In the 1440s, the Mongols once again became a threat and Japanese pirates, known as wokou, became an increasing menace. In the seventeenth century, the Manchus began to gather power over an already weakened country, and would eventually form the Qing Dynasty. During the later period of the Ming, Western culture flooded into China. A number of Jesuits arrived bringing with them their religion, philosophies and knowledge. Matteo Ricci , the famous Italian Jesuit missionary scholar, was to develop a close relationship with Chinese scholars. Different Schools of Medicine
The work of many eminent physicians and the publication of numerous treatises testify to the blossoming of medical theories and practices during the Ming period. Despite this, Chinese medicine continued to rely mostly on the medical classics and many Ming handbooks drew on these. Following the Jin and Yuan dynasties, there were great debates among physicians from the different schools advocating different philosophies of Chinese medicine. The three major schools in this period were the school of nourishing the yin, the school of warming and invigoration, and the school of epidemic disease.School of Nourishing the Yin
The founder of this school was Zhu Zhenheng, whose theory was aimed at nourishing the yin and quenching the minister fire. Two famous doctors, Wang Lu and Dai Sigong , became disciples of this school and continued to advocate, as a Ming therapeutic approach, Zhu Zhenheng's theory in their practice. The School of Warming and Invigoration
Although the schools of medical thought founded by Zhu Zhenheng had their followers during the Ming dynasty, many physicians supported the ideas of the "school of warming and invigoration" (wenbu) founded by Li Gao. They believed that tonifying the spleen and stomach preserved the vital energy (qi) and kept away illness. The foremost physicians in this area of thought were Xue Ji, Zhao Xianke and Zhang Jiebin.Xue Ji (c. 1488-1558), whose father had been a member of the official Academy of Medicine, was a specialist in internal medicine, surgery, gynecology, pediatrics and otorhinolaryngology. He published a wide variety of medical classics, including Neike Zhaiyao (A Summary of Internal Medicine), Waike Shuyao (Essentials of External Medicine), Waike Fahui (The Development of External Medicine), Nuke Cuoyao (A Resume of Gynecology), Zhengti Leiyao (A Repertory of Traumatology), and Kouchi Leiyao (A Repertory of Stomatology), providing ample testimony to his medical interests. He also recommended decoctions to treat poor appetite and fatigue which were described as being able to "regulate or invigorate the middle burner and increase energy," in the book of Piweilun (Treatise on the Spleen and Stomach) by Li Gao and commonly made use of atractylodes rhizome, ginseng, liquorice and milkvetch root. Zhao Xianke developed the teachings of Xue Ji to formulate the theory of the "gate of vitality" (mingmen). According to Zhao, it was this "gate of vitality," located between the kidneys, rather than the heart that governed the body. The amount of "fire" generated by this gate determined the degree of available energy. Zhao believed in a relationship between fire (yang) and water (yin). Nourishment of one or the other was the basis for his treatment and to achieve this he gave his patients one of two pills: "the pill of eight ingredients" to reinvigorate fire (yang), and "the pill of six ingredients" to reinvigorate water(yin)." The prescriptions for these were taken from the text written by Zhang Zhongjing in the second century AD, Jingkui Yaolue (Summary from the Golden Chest).Another notable medical commentator of the time was Zhang Jiebin (1563-1640), also known as Zhang Jingyue. He disagreed with Zhu Zhengheng that yang was generally excessive whilst yin was insufficient, believing instead that yang was the source of life and the root of our physical existence. He wrote many works aimed at explaining and simplifying the ancient classic Huangdi Nei Jing (The Yellow Emperor's Classic of Internal Medicine).The School of Epidemic Disease (wenbing)
Prior to the Ming dynasty, febrile illness (wenbing) or cold-induced illness (shanghan) were the general names for acute feverish disease caused by exogenous pathogens. The terms covered both infectious and non-infectious diseases. It was only at the beginning of the Ming dynasty that the precise features and a definition of wenbing were formulated. Wang Lu was the first physician to clearly define different approaches to the treatment of shanghan and wenbing. Wenbing became the name for cases of infectious disease only.

Wu Youxing ( 1580-1660) |
Plague was a major problem during the Ming period and was spoken of as wenyi (pestilence), that is any kind of fatal epidemic disease. An outbreak in 1641 wiped out a large portion of the population in China. The physician Wu Youxing (c. 1580-1660) made an important breakthrough on wenbing. After extensive research into epidemic disease, he published a book Wenyilun (On Pestilence) in 1642. In this, he described the specific symptoms of different kinds of epidemic disease and proposed the theory of liqi (excessive influences). His theory of liqi stated that pestilence was not caused by exogenous pathogens (such as wind, cold, summer-heat and wet), but was the result of infection by excessive influences. Liqi had the following characteristics: | * | It could be cured by herbs. |
| * | Penetration of the body took place through the mouth and nose. |
| * | Occurrence of disease depended on the quantity and virulence of the excessive influence, and body resistance. |
| * | Each pestilence was associated with its own particular liqi. |
Wu Youxing also claimed that the liqi affecting humans was different from that occurring in animals. He suggested that liqi was the cause of smallpox and other inflammatory skin diseases. Smallpox was a great scourge of the country during the Ming dynasty and there is documented use of anti-smallpox vaccination dating from the years 1567-72. Advancement in Surgery
Various other new medical ideas arose during the Ming. The concept that internal and external treatment should be combined to tackle illness was shared by several physicians and surgeons. The theory was extended to the treatment of cancer by a number of practitioners who recognized contributory causative factors, such as depression and the eating of fried, spicy or charred food. The development during the Ming of methods for achieving analgesia (pain relief), asepsis (absence of illness causing organisms) and hemostasis (the arrest of bleeding) contributed to an improvement in surgical technique. 
Waike Zhengzong
(The Genuine Surgery) |
Chen Shigong (1555-1636) was one of the outstanding surgical figures of this time. He dedicated himself to external medicine for over 40 years. His Waike Zhengzong (The Genuine Surgery), first published in 1617, covered a series of surgically treatable diseases and many effective prescriptions. The book outlined the surgical procedure for the repair of a slashed throat, the use of copper wire to excise nasal polyps under local anesthesia, and described in detail cancer of the lip and breast. These were the earliest surgical records in TCM history.
Ravages of Venereal Disease
The cleanliness of the sexual habits observed by the Chinese was thwarted during the sixteenth and seventeenth centuries by outbreaks of syphilis that ravaged the country. The disease appears to have spread from the southern coastal region of Canton. Physicians of the period devoted much effort to combating syphilis and two notables were Wang Ji and Chen Sicheng.Wang Ji (1463-1539) held the view that a combination of internal and external therapy was needed to deal with venereal disease and prescribed a "decoction of the four rulers" (ginseng, large head atractylodes root, Indian bread and liquorice root) to sustain vital energy (qi), while applying an ointment containing honeysuckle to the lesions. At times he cauterized the ulcers using garlic. To complete recovery, he gave a further decoction, which in addition to the ingredients used in the "four rulers" contained rehmannia root, peony root, chinese angelica and szechwan lovage rhizome. This remedy is still in use in Chinese medicine as a tonic for qi and blood. Chen Sicheng, who lived about 100 years after Wang Ji, devoted an entire work to the treatment of syphilis. His Meichuang Milu (Secret Writings on Putrid Ulcers) published in 1632 was the first of its kind in China. The book suggested prescribing arsenic and mercury to cure syphilis. This preceded their use in Western medicine by about three hundred years.Promotion of Acupuncture
Acupuncture and moxabustion continued to be widely used and studied under the Ming. In 1443, the Ming government ordered the casting of a bronze statue marked with the acupuncture points after the one produced in the Song dynasty. Yang Jizhou (1522-1620) published the most significant text of the period on acupuncture, Zhengjiu Dacheng (The Great Success of Acupuncture and Moxabustion). The book gathered important information from previous texts and enjoyed much popularity within the medical community. It was regularly reprinted in subsequent centuries. Pharmacopoeias and Prescription Books
The Bencao Gangmu (Compendium of Materia Medica)
One of the most prolific writers and innovative medical practitioners of the Ming period was Li Shizhen (1518-93). A native of Qizhou, he was born into a family of physicians, the vocation often passing down in families for generations. 
The Bencao Gangmu (Compendium of Materia Medica) - was translated into different languages |
Of the seventeen works that Li published, the Bencao Gangmu (Compendium of Materia Medica) is perhaps the most well known and regarded. Li Shizhen used Tang Shenwei's work Zhenglei Bencao (Classified Materia Medica) as a reference. He revised the classification of drugs, expanded the list of known drugs, corrected previous errors, and created guidelines for the collection, preparation and use of drugs. Li unveiled 374 new drugs in his text in a list of 1,892 and included over 1,000 illustrations. The book summarized most of drug information available in the sixteenth entury.
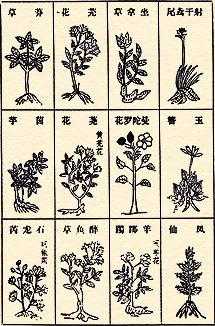
Illustrations form the Bencao Gangmu (Compendium of Materia Medica) |
Classification in the Bencao Gangmu (Compendium of Materia Medica) differed from previous materia medica by listing drugs under 16 headings:
| 1. Water | 9. | Fruit | | 2. Fire | 10. | Tree | | 3. Earth | 11. | Products derived from 'garments and tools' | | 4. Metal | 12. | Insect creatures with scales (reptiles, fish) | | 5. Stone | 13. | Creatures with shells | | 6. Plant | 14. | Bird | | 7. Cereal | 15. | Quadruped | | 8. Vegetable | 16. | Products of human origin |
|
These headings were further subdivided. Plants were organized under their habitat or special character and to some extent Li anticipated the concept of a "plant family." Previous materia medica had been organized by toxicity or by the somewhat arbitrary origins of substances. Li was also a well-respected physician and maintained a critical approach in his work. He believed that the mind had an important influence on the body. He was the first in China to identify gallstones, he used ice to reduce fever and developed techniques of disinfection. He attached greater attention in his work to the prevention of illness rather than to its cure. By the end of his career, he had a reputation as a herbalist, pharmacologist and physician, and also as a botanist, zoologist and mineralogist. He was a great humanitarian, promoting the Confucian principle that care should be extended to everyone. Prescription Monographs
Standards for the combination, pharmacology, efficacy and administration of herbal prescription were improved during the time of the Ming. Many texts were published, including in 1406 the largest ancient Chinese prescription book, the Puji Fang (Prescriptions for Saving the Public). Zhu Su and Teng Shuo edited this book, listing 61,739 prescriptions with 239 illustrations. They gathered a wide variety of prescriptions and folk remedies, preserving most of the previous records of herbal use for future generations.  |
| Emperor Kangxi (1662-1722) |
The Qing Dynasty 1644 - 1911 AD About the Qing Much weakened by long wars with the Mongols and harassment by Japan, the Ming dynasty was brought to a close in 1644 by the
Manchu chieftains. To prevent internal conflict, the Qing pursued in certain circumstances a policy of giving rewards of land for cultivation and reducing or exempting taxes. The early Qing emperors, especially Kangxi (1662-1722 ), Yongzheng (1723-35) and Qianlong (1736-96), not only resolved the long conflict between nomads and peasants which had plagued China throughout its history, but also undertook a series of measures to develop the economy, culture and transportation in the frontier areas. As a result, they consolidated national unification and laid the foundation for modern China's territorial boundaries.
 |
| Map of Qing Dynasty |
In spite of these noticeable achievements, the Qing rulers were autocratic and despotic. The nation was still agriculturally based and dominated by feudal ethics and rites. Worse still, the Qing empire in its relationship with foreign countries was isolationist, conservative and arrogant. It paled in comparison with the newly industrialized West and was left behind in world development. The gap between China and the West gradually widened.
During the mid-Qing dynasty, social conflict began to surface. Many revolts took place and that of the White Lotus Sect put an end to the Qing's golden age. The Opium War of 1840 and increasing foreign aggression resulted in many unequal treaties being signed between the Qing and Western imperialist powers. All these treaties demanded that China cede territories, pay indemnities and/or open trading ports. Eventually, China became a semi-feudal and semi-colonized country. With its corrupt politics and conservatism, the Qing dynasty rapidly declined. The dynasty was finally overthrown by the Revolution of 1911 led by
Dr. Sun Yat-sen.
Ye Gui (1667-1746) |
Further Development on Febrile DiseaseIn the Ming dynasty, Wu Youxing's
Weiyilun (On Pestilence) of 1642 exerted considerable influence on what is known as the
"school of febrile illness" (wenbing). Wenrebing which was derived from "wenbing", were diseases associated with heat, which today remains one of the disease causing agents of TCM. Through clinical practice and further study, physicians in the Qing dynasty gave new prominence to the study of wenbing. The most significant representatives of this school included
Ye Gui ,
Xue Xue and
Wu Tang. Wang Mengying (1808-66) devoted an entire work to fever-related illnesses, the
Wenre Jingwe.
Wenre Fengyuan (The Source of Fevers) by Liu Baoyi (1842-1901) and
Shibinglun (Seasonal Illnesses) by Lei Feng in 1882 also exerted a lasting influence in this area.
Confronted by the challenge of Western medicine, the practice of Chinese medicine was buttressed by its long-held traditions and continued unabated in the later-Qing period. Its survival was assured by the adherents to the
Shanghanlun (Treatise on Febrile Diseases),
school of "cooling",
the Shennong Bencaojing (Classic of Herbal Medicine) and other champions of traditional Chinese medicine.
New AnatomyChinese anatomy continued to rely essentially on the information provided in the
Huang Di Nei Jing (The Yellow Emperor's Medicine Classic). Little had been added to this work since its completion because surgery had not been looked upon favorably over the centuries.
Wang Qingren (1768-1831) |
Although it was not the first documentation of proper anatomy, Wang Qingren (1768-1831) published his
Yilin Gaicuo (Errors Corrected from the Forest of Physicians) in 1830. In this, he dispelled certain long-held beliefs, such as the claim that urine originated from excrement and that the lungs had 24 holes. His observations from corpses abandoned in public cemeteries and execution grounds led him to discover organs and structures previously unmentioned in traditional Chinese medicine. These included the abdominal aorta, pancreas and diaphragm. He also showed that it was the brain and not the heart, as was previously thought, that was the seat of thought and memory.
Use of the Smallpox Virus to Combat SmallpoxPrevention measures for variola (smallpox) had been used in China as early as the sixteenth century, during the time of the Ming. According to Yu Maokun, whose
Douke Jinjing Fujijie was published in 1727, variolation (inoculation against smallpox) had been practiced since the years 1567-72. The method involved extracting the dry scabs caused by the disease, reducing them to a fine powder and then having the patient inhale the powder through the nose with the aid of a silver tube. Despite the imperfection of such a method, it is undeniable that variolation as practiced in China played a significant role in the prevention of smallpox. It was the earliest vaccination method in the world. Knowledge of the process quickly spread to Europe.
Supplement to the Bencao Gangmu and Plant TherapyZhao Xuemin (1719-1805) bequeathed to Chinese medicine and pharmacy a supplement text to the
Bencao Gangmu (Compendium of Materia Medica),
called Bencao Gangmu Shiyi, published in 1765. A total of 921 drugs were listed under the categories of water, fire, earth, metals, stones, herbs, trees, creeping plants, flowers, fruit, seeds, vegetables, utensils, birds, quadrupeds, creatures with scales or shells, and insects.
The most significant feature of Zhao's work, however, was the introduction of medical substances that he had learned to recognize and use while talking with traveling physicians. His book,
Chuanya (1759), recorded these teachings. The popularity of such physicians, who were also known as "bell physicians"
(lingyi) because they announced their presence by means of a small bell, stemmed from the fact that they prescribed medicinal plants that were accessible and thus inexpensive. Zhao Xuemin thought highly of these physicians (it might be said that the famous "barefoot doctors" of post-1949 China were their heirs), concluding that the drugs they recommended were cheap, efficient and practical. He noted in the book that drugs need not be expensive and berated the medical quacks whose scientific skills did not match their high fees. In his opinion, such people knew how to prescribe an expensive tonic, but did not know how to recognize a medicinal plant.

The traveling herbalist in Qing
(Taken from the Complete Illustrated Guide to Chinese Medicine, 1996 ) |
Typical Chinese dispensary
(Taken from Chinese Herbal Medicine 1986) |
Phytotherapy (plant therapy) remained the basis of Chinese medicine throughout the nineteenth century and earlier medical works of this tradition were reissued in new editions. It was the desire to revive this plant-based medicine that inspired physicians like Wu Qijun (1789-1846), who published
Zhiwu Mingshi Tukao (Illustrated Account of Flora), and Fei Boxiong, who published
Yichun Shengui in 1863. The best known dispensary of the time, the
Tongren tang, was located in the capital Beijing and catered especially to the imperial family.
Publishing Boom in Encyclopedias and Medical Books Anxious to obtain the support of the scholar class, the new rulers encouraged intellectual life and gave patronage to encyclopedic projects in history, arts, medicine and science.

Illustrations from Yizong Jinjian
(Golden Mirror of Medicine)- about bone setting |
The encyclopedia became very popular in the 1700s. One Chinese medicine classic that emerged during this publishing boom was the
Gujin Tushu Jicheng (Collection of Ancient and Modern Works), an encyclopedia of 10,000 chapters that provides much background to the history of Chinese medicine. Published in 1726, about 520 chapters of the encyclopedia focused on medicine. Another famous work was the
Yizong Jinjian (Golden Mirror of Medicine) written by Wu Qian in 1742. To this day, this remains an important reference book.
A trend also developed of authors writing collections of books. These collections provide windows into the different thoughts of the period. For example, Zhang Lu (1617-1700) wrote
Zhangshi Yitong (A Summary of Master Zhang's Medical Thought), which supported the
school of warming and invigoration.
At the same time, more modest publications on medicine appeared. They tended to be introductions into Chinese medicine, such as the
Yixue Xinwu ( An Understanding of Medicine) published in 1732 by Cheng Guopend. The book discussed the four methods of examination, diagnostic principles and therapeutic techniques that served as the basis of medical training. Another book,
Zhengzhi huibu by Li Yongcui, which dates from 1687, is entirely devoted to illnesses and their symptoms that relied on internal medicine for treatment.
The fascination for ancient classics re-emerged during the Qing period and many were re-edited, such as the
Huang Di Nei jing (The Yellow Emperor's Medicine Classic),
Shanghanlun (Treatise on Febrile Diseases) and
Jinkui Yaolue (Summary of the Golden Chest). They enjoyed considerable popularity and were subject to various commentaries.
Other texts written during this dynasty focused on topics such as gynecology, pediatrics, ophthalmology, massage and external medicine, which mainly dealt with skin diseases or trauma.
Rise of Western Medicine China's internal weaknesses made her vulnerable to Western nations hungry for economic benefit in the later nineteenth century. Christian missionaries and medical doctors associated with the church played a major role in establishing foreign influence in China at this time. This triggered growth in the number of medical schools run by the Chinese, or jointly with Western doctors, and many Western medical books were translated. Chinese doctors at this time were also introduced to Western medical practice. The first Chinese to study medicine abroad was Huang Kuan (1829-1878), a Cantonese who went to Edinburgh University in Scotland, and then disseminated what he had learned on returning to his native Guangzhou. This brought about a new generation of doctors who saw a wealth of knowledge in Western medicine.

A description of ginseng which talks about its properties and functions. Ginseng was an expensive herb even in the Qing Dynasty and hard to come by. |
Integrated Traditional Chinese MedicineIn the late-Qing, this Westernization movement had a significant impact on traditional Chinese medicine. Response to the movement varied: some practitioners refused to accept Western medicine, denying its value completely; some regarded traditional Chinese medicine as non-scientific and argued that it should be banned; and others tried to learn from Western medicine and integrate this knowledge into their traditional practice. One of the earliest pioneers for the integration of Eastern and Western medicine was Zhu Peiwen. His
Huayang Zangxiang Yuezuan (A Combining Chinese and Western Anatomy Illustration) of 1892, illustrated organs according to both Chinese and Western concepts. He suggested that each tradition had its advantages and disadvantages. This integrated approach enjoyed little success during the Qing dynasty because of strong adherence to traditional Chinese medicine texts and skepticism about medical knowledge garnered from the West.
Modern China 1912AD ~ PresentAbout Modern ChinaThis period in Chinese history presented enormous challenges for Chinese medicine. The rapidly changing political environment, combined with much foreign influence, altered perceptions of medicine generally. These perceptions both hindered and advanced the practice of Chinese medicine and led to the system that is current in China today, where Chinese and Western medicine are practiced side by side for the benefit of the patient.
National Flag of Republic of China |
The 1911 Revolution to Mao Zedong and Communism
The Qing Dynasty finally collapsed in 1911 as a result of the might of the Kuomingtang, led by
Sun Yat Sen. A republic was formed in January 1912 and the capital moved from Beijing to Nanjing. However, the new government was unable to consolidate its power in China. Warlords (many of whom were part of the military under Sun Yat Sen) reappeared and exerted rule in many small areas of the countryside.
Foreign powers, such as the English, French and Americans, who had previously negotiated unfair trade deals under the Qing Dynasty, cheated China of her cultural heritage and further weakened her sovereignty. Their presence allowed Western concepts, especially those pertaining to medicine, to slowly pervade the country and by the 1900s Western ideas were embraced as a means to modernize the country. The practice of Western medicine was in large part brought to China in the 1800s by
missionaries, who set up hospitals and dispensed Western medicines. The trade deals negotiated by these foreign countries protected the missionaries and fostered the spread of Western medicine.

Map of Modern China |
Chiang Kaishek eventually reformed Sun Yat Sen's government under the National People's Party. This new Kuomingtang (KMT) government came to power in Nanjing in 1927 and achieved a temporary unity in the country. The Chinese Communist Party, established in 1921, was the opposing political force during that time. In 1931, shortly after these two parties came into being, Japan invaded Manchuria and started a war that lasted eight years. These eight years of
Japanese occupation had devastating effects for China.

Flag of People's Republic of China |
After the Japanese surrender, conflicts between the two political parties escalated into civil war. Mao Zedong led the People's Liberation Army against the KMT nationalists. Initially, Mao Zedong was forced to retreat to the Yanan area, but eventually he was successful in gaining control of the entire country, forcing Chiang Kaishek and his followers to retreat to Taiwan. In 1949, the People's Republic of China (PRC) was established with Mao Zedong as its chairman. The capital was moved back to Beijing. This time the government was able to achieve lasting unification of the country, although the Chinese people still faced much hardship.
The Health Problems of China and a Divergence from Chinese Medicine
In the first half of the 20
th century, the health of the Chinese population suffered greatly. Epidemics were rampant and diseases such as
cholera,
plague, smallpox,
black fever,
diphtheria,
scarlet fever, malaria,
bilharzia and tuberculosis caused hundreds of thousands of deaths. People were further plagued with famines and unremitting starvation.
The famous cartoon features - Sanmao, in which the sanitary conditions of early modern China are described. |
Perhaps it was as a result of these horrific conditions, combined with the changing political climate, that more emphasis was centered on public hygiene and government leaders began to show a preference for Western medicine over
Traditional Chinese Medicine (TCM). More regulations for medical education were put in place and an increase in health centers staffed by Western and Japanese doctors was seen together with a surge in the numbers of professional medical associations and journals.
To some extent, Chinese medicine became a symbol of the old backward ways of doing things to those who wished to modernize China. Wang Daxie, who was the Minister of Education in Sun Yat Sen's government, was one of the first officials to call for the abolition of Chinese medicine. Although he was not successful in this, the new nationalist Kuomingtang government adopted similar views about Chinese medicine. A proposal entitled "
A Case for the Abolishment of the Old Medicine to Thoroughly Eliminate Public Health Obstacles," written by Yu Ai and Wang Qizang, suggested that important Chinese medicine principles, such as the yin yang theory and the five elements, were not based on reality and further intimated that Chinese medicine was fraudulent. The proposal, which was passed by the Central Ministry of Health in 1929, severely limited the advertising and practice of Chinese medicine. It also prohibited anyone from establishing Chinese medicine schools, so that the spread of "unscientific" information could be controlled.
A sample Chinese medicine advertisement: The advertisement boasts of 32 secret prescriptions from famous physicians of past & present to cure 32 ailments. |
Even Mao Zedong, who was leading his Red Army in the Yanan area at the time, mirrored the Nationalist government sentiments. Both his army and the surrounding population were experiencing a shortage of food, shelter and clothing, and faced additional problems of illness due to poor hygiene and sanitation. This prompted him to instruct his army in 1942 to uproot all "shamanic beliefs and superstitions"
5 and form model public health villages. Proper hygiene and sanitation remained of prime concern to him and like his nationalist counterparts he thought Chinese medicine doctors were no better than "circus entertainers, snake oil salesman or street hawkers."
6Despite all the negative sentiment about Chinese medicine during this period, its practice was
impossible to eradicate. Yu Ai and Wan Qizang's proposal sparked heavy protest from the Chinese medicine communities. In March 1929, members of 132 TCM associations congregated in Shanghai and the National Union of Associations for Chinese Medicine was formed. From that day forward, March 17th was declared the birthday of Chinese medicine.
Integration and Modernization of TCMDespite the debate over official government policy and attitude, TCM was still widely accepted and used among the common people, especially in the countryside where the majority of China's ballooning population lived. With the growth of Western medicine in China, many TCM physicians saw the benefit of assimilating it into the practice of TCM. As a result, a new school of thought, referred to as zhongxi huitong pai or "School of Sino-Western Convergence and Intercourse," emerged. The following are important figures that followed this school of thought.
| Tang Zonghai (1846-1897) is considered the forefather of convergence. A native of Sichuan, he had the benefit of studying both Chinese and Western medicine. In his 1892 book, Zhongxi Huitomg Yijing Jingyi, he supported convergence and urged each side to overcome any shortcomings and form one system. He listed the advantages and disadvantages of each system, and was a great supporter of Chinese-Western medical exchange. Zhang Binglin was not only a supporter of the school of convergence, but was also a political activist. He met Sun Yat Sen in 1899 while in Japan and became a member of Sun's Alliance League. In his controversial writings, which won the attention of well-known writers such as Lu Xun, he supported the adoption and acceptance of Western scientific theories. |
Of course, there were many other medical practitioners who thought that the best way of preserving Chinese medicine was to incorporate Western views into its practice. Other important figures such as
Yun Tieqiao,
Yang Zemin,
Fu Lanyuan,
Ding Ganren, Zhang Shanlei, Xie Liheng,
He Lianchen and
Qiu Jisheng also contributed to the advancement of Chinese medicine during this time.

Map of Modern China and Taiwan |
Mao Zedong and Chinese MedicineWhen Mao Zedong, the Great Helmsman, drove the Kuomingtang out of China in 1949, the anti-Chinese medicine stance continued until after the Kuomingtang had fled into what is today known as Taiwan.
In 1942, Mao had ordered the government to banish all superstitious and shamanic beliefs from the Yanan region and to create public health villages. However, in the years between 1953 and 1959, well before the Cultural Revolution was launched, Mao reversed his anti-Chinese medicine stance. Chinese medicine was used as a symbol for China and considered a national treasure by the government.
Historically, these are the years when the leader was most hungry to gain power and influence in the communist world. During this period Russia, as the former Soviet Union, was quickly gaining global power and recognition. Russia was soon perceived as a threat and possible superpower alongside the United States. Mao was keen to create a form of communism that would put him and China in the spotlight amongst communist countries, and at the same time diminish China's growing reliance and dependency on the Soviets. (China actively depended on the Soviet Union for medical equipment and pharmaceutical drugs.) The kind of communism Mao set out to create focused on "patriotism," "being self reliant" and "native." Chinese medicine promoted this form of communism.
As a result, there was a revival of Chinese medicine during these years. In 1954, the Department of Chinese Medicine was established under the Ministry of Public Health (Oriental Medicine). Thanks to Mao's endorsement, institutions, such as the Shanghai College of TCM, Beijing College of TCM, Chengdu College of TCM, Guangzhou College of TCM and Nanjing College of TCM, were established. Leading by example, Mao himself would use a traditional Chinese medicine remedy called "yin qiao san" and allow two important TCM practitioners Li Shizhi and Peng Luxiang of the Chengdu College of TCM to be present at his bedside when he fell ill during a
Great Leap Forward conference in Chengdu in 1957.
Mao's Policy of Integration of East and West MedicineIn 1958, at the beginning of Mao's Great Leap Forward campaign, the practice of Chinese medicine again experienced more changes. Mao revealed his vision of
zhong xi yi jiehe, which translates as the "integration of Eastern and Western medicine." His idea was to insert some of the rigor of modern science into Chinese medicine's future development. This led to a search for 2,000 Chinese physicians highly trained in Western medicine to attend special seminars dedicated to the study of Chinese medicine over a two-year period. Only about 200 physicians graduated from this program, a possible testament to the fact that the study of Chinese medicine was difficult. Many of these doctors became top administrators in the 1980s and 1990s, as China once again sought to open its doors to both Eastern and Western thought after the tumultuous years of the Cultural Revolution. Mao's integration policy also led to the establishment of TCM in in- and out-patient departments in hospitals and TCM education was restructured to include some Western medicine instruction. Many patients turned to TCM treatments when Western therapies were not successful.
The Cultural RevolutionThe Cultural Revolution (1966-1976) was used by Mao Zedong to try to regain power and influence in the political arena and he played on the sensitivities of the masses to achieve this. As a result, traditional culture, thinking and perspectives were crushed. Academics, professors, doctors and those who were well educated became targets of the campaign, while farmers, laborers and the uneducated gained power and influence during these years.
The purpose of the revolution is questioned to this day and is frequently debated, but the damage that it did to ordinary people and to higher education was extraordinary. Between the years 1966 and 1971 no new students were permitted to enter any academic institution. Schools were shut down and hundreds of thousands of youths were sent into the countryside to become indoctrinated or re-educated according to Mao's principles. Others became "red guards" and traveled the cities and villages smashing whatever and whoever was associated with tradition. Artifacts, temples and churches were demolished; literature was burned; teachers were ridiculed; and the educated mocked, forced to write apologies and sent to indoctrination camps.
The key word in this revolution was "reform" and Mao had specific views on how that reform would be acted out for healthcare. In a speech to healthcare professionals in Beijing on 26 June 1965, he stressed the need to reform medical education: "It is completely unnecessary to engage in so much studying. How many years of formal education, after all, did
Hua Tuo have? And how many
Li Shizhen. There is no need to restrict medical education to people with high school diplomas; middle school and elementary school pupils studying for three years will do. If this type of lowly educated doctor is then sent to the countryside, he will always be able to do a better job than the charlatan shamans; and the peasants, moreover, will be able to afford such care." Mao ended the speech with this bluntly stated viewpoint: "Studying is a stupid endeavor for a doctor."
7  A statue of a barefoot doctor A statue of a barefoot doctor |
Con sequently, the old medical curriculum was buried and the most revered medical practitioners were killed, imprisoned or sent to indoctrination camps for their "traditional" ways of thinking. The doors of learning were now opened to workers, peasants, soldiers and other members of the under-privileged classes. Entrance exams were scrapped, admission was based on family background and political status, and textbooks were filled with quotes from Mao's collected works and "little red book." Those passing through this system received minimal training in Western and Chinese medicine. This movement provided the bulk of the "barefoot doctors," who had very limited medical knowledge, but served a major role in addressing medical needs in the countryside. In fact, the barefoot doctors had already begun to emerge in the 1950s and most were young villagers. Their importance cannot be under-estimated since they attended the needs of a nation where over 90 per cent of the population lived in the countryside. By 1984, there were some 1.28 million barefoot doctors practicing in China.
Chinese medicine practitioners also suffered greatly under this movement. One prominent leader in Chinese medicine, Ren Yingqiu, was banished to the Qing Hai Province (
an area likened to Siberia) and was allowed to bring only one book. This was Li Shizen's pharmacopeia
(Bencao Gangmu). The class of 1963 was the last class to complete a full TCM curriculum. No students were admitted into Chinese medicine schools during the years between 1965 and 1970.
After the Cultural Revolution was officially ended in 1976 with the death of Mao, academics, artists, professionals, and TCM and Western physicians slowly re-emerged into society.
Modern Chinese Research and Development 
Patent Chinese medicine in pills, capsules and liquid forms |
Despite the problems that were faced by Chinese medicine during the 20th century, research was carried out not only in Western medicine, but also in the use of Chinese medicinal herbs and many technological advances were made. As early as the 1920s, pharmaceutical research in China became more systematic. This was due to the influence of graduates from European, American and Japanese universities who applied their scientific knowledge in Chinese laboratories. During the 1930s and 1940s, the Central Research Institute, the Beijing Research Institute and the Central Laboratory of Hygiene focused on the therapeutic quality of plants such as
Szechwan lovage rhizome, plantain seed, pinellia tuber, rehmannia root, tangshen and, in particular, the antifebrile
dichroa root, which had been traditionally used to combat malaria. Chemical, clinical, pharmacological and parasitological research further validated the use of this plant as an antimalarial agent. Naturally, these research activities generated a variety of publications describing the application of traditional herbs in modern medicine. One of the most important of these was the
Zhongguo Yaoxue Dacidian (Chinese Pharmaceutical Encyclopedia), which was published by Chen Cunren in the early 1930s. After the People's Republic of China was founded, the preservation of China's traditional herbs became a priority. There are an estimated 4,000-5,000 medicinal herbs growing in China of which 1,000 are commonly used. Measures have been taken to research their optimal growing conditions and to stimulate production. Some herbs are now grown systematically on plantations, as opposed to forest collection, with many of the large-scale enterprises following good agricultural practice (GAP). Other advancements made in the last century include modification of the dosage forms. Chinese medicine is now available not only as traditional decoctions, but also in the form of pills, tablets, capsules, granules, suppositories, creams, lotions and suspensions. This provides a more accessible and user-friendly form of medication. Other Chinese medicines are prepared for intravenous use in hospitals.
Some notable achievements which have resulted from the combination of Eastern and Western medicine during this century include the setting of fractures with mobile willow twig splints after determining the nature of the break using X-rays; the use of acupuncture anesthesia during surgery; and the performance of taijiquan (better known as tai-chi, a traditional Chinese exercise) to build up the body's immunity and help prevent certain chronic illnesses.
Chinese Medicine Today 
Teaching class of Shanghai University of Traditional Chinese Medicine |
Today, medicine in China focuses very much on integration, seeking a fusion of East and West. The challenge is to extract the best from both systems to maximize the benefit for the patient. Health statistics have shown that the practice of both Western medicine and TCM has grown rapidly. According to the 1991 Chinese Health Statistical Digest, the number of Western-trained doctors soared from 3,800 in 1949 to 1.1 million in 1991; and over the same period, the number of doctors practicing TCM rose from 27,600 to 362,600. The number of hospital beds provided for both systems has also risen. Hospital beds available for TCM increased from a mere 220 in 1949 to 188,200 in 1991, while those for Western medicine rose from 84,400 to 836,360. A three-tiered system - a blend of TCM, Western and integrated medicine - has emerged which offers patients better healthcare choices than any one of the systems alone. As Chinese medicine gains more popularity in the West, China will continue to move forward with research and education. This will further TCM's development and practice and serve as an important resource for those who wish to share in its bountiful benefits.










































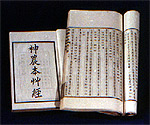




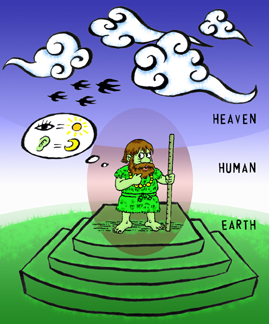




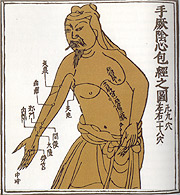

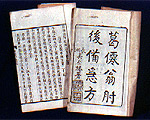








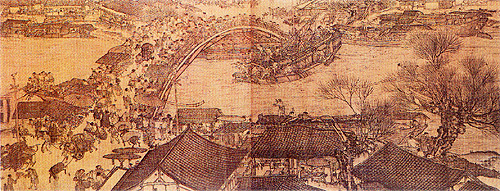


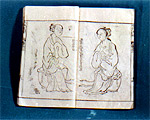
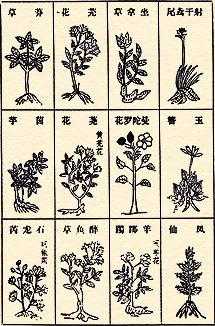






 A statue of a barefoot doctor
A statue of a barefoot doctor